Insulin is a hormone made by the pancreas. It acts like a key that opens the door to the body’s cells. Sugar can then move out of the blood and into the cells to be used for energy. Insulin keeps the sugar in your blood under control.
There are 3 types of diabetes:
- Type 1: People do not make insulin.
- Type 2 and gestational: People become resistant to insulin, and it does not work to keep their blood sugar under control.
The major side effect of taking insulin is a possible low blood sugar.
Types of insulin
Below are the main types of insulin used during pregnancy.
Rapid-acting insulins: Aspart (Novolog®) and Lispro (Humalog®)

- Works in 15 minutes
- Peaks in 1 to 2 hours
- Stays in your body for 3 to 4 hours
- Looks clear
Intermediate-acting insulin: NPH (Humulin® N or Novolin® N)
- Works in 2 to 4 hours
- Peaks in 4 to 10 hours
- Stays in your body for 10 to16 hours
- Looks cloudy
Insulin storage
These types of insulin can be stored at room temperature for 28 days after opening. Keep unopened bottles and pens in the front of your refrigerator.
Doses
Humalog/Novolog *** units before breakfast
*** units before lunch
*** units before supper
Humalin N/Novolin *** units before breakfast
*** units before bed
How do I draw up insulin using a vial?
- Wash your hands with soap and water.
- Gather your supplies:
- Insulin vial
- Syringe
- Alcohol pad
- Mix the intermediate-acting insulin (NPH) by rolling the bottle gently in the palms of your hands. You can also turn the bottle upside down at least 10 times. Do not shake the bottle. Mix it more if a white layer is still at the bottom of the bottle of insulin vial.
Clean the rubber stopper with the alcohol pad.
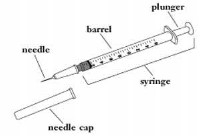
- Pull back on the plunger to fill the barrel with air by:
- Taking the needle cap off the syringe.
- Pointing the needle up.
- Pulling back to your ordered dose of insulin.
- Push the air into insulin vial by:
- Pointing the needle down.
- Pushing the needle straight into rubber stopper on the vial.
- Pushing the plunger down until all the air has been pushed into the vial.
- Draw up your insulin dose.
- Keep the needle in vial.
- Turn the vial upside down so the needle is pointed up and the rubber stopper is down.
- Pull down on the plunger to fill the barrel with the dose your doctor ordered.
- Make sure there are no air bubbles in syringe.
How do I give myself an injection?
- Wipe the injection site with alcohol or soap and water.
- Hold the syringe straight up and down and push the needle into the injection site at a 90-degree angle. Be sure the needle is all the way in your body.
- Push down the plunger at a steady rate until the syringe is empty.
- Pull the needle out of your body.
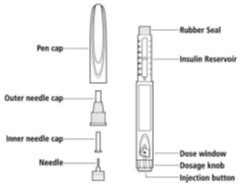 Using an insulin pen
Using an insulin pen
- Take the pen cap off and put a new needle on the pen.
- Take off the paper tab.
- Push the needle onto the top of the pen.
- Twist on the needle. Do not over tighten.
- Take off the outer needle cap. Do not throw away. Then, pull off the inner needle cap and throw away.
- Take off the outer needle cap. Do not throw away. Then, pull off the inner needle cap and throw away.
- Do a safety test to make sure all air bubbles are out of the needle.
- Turn the dose knob on the end of the pen to the first 1 or 2 clicks.
- Hold the pen with the needle pointing up.
- Push the injection button.
- Look at the needle to be sure fluid comes out.
- Repeat if needed, until a drop appears. It may take several tries to see fluid come out of a new pen.
- Check the dose window to be sure you see “0” in the dose window.
- Mix the intermediate-acting insulin (NPH) by rolling the pen gently in the palms of your hands. You can also turn the pen upside down at least 10 times. Do not shake the pen.
- Turn the dose knob to your insulin dose.
- Choose an injection site. Then, clean the site with an alcohol swab or soap, water, and a paper towel. Let the site dry.
- To reduce the risk of infection at the site, do not touch the uncapped needle with anything. If this happens, use a new needle.
- Push the needle into the skin at a 90-degree angle. Be sure the needle is all the way in your body.
- Push down and hold the injection button until it stops. Hold it for 5 to 10 seconds. Make sure you see “0” in the dose window.
- Pull the needle out of your body.
- Cover the needle with the outer needle cap. Twist off the needle. Put the used needle in a medical sharp or puncture-proof container, such as a liquid detergent bottle.
- Put the pen cap back on the pen.
Where can I inject insulin when I'm pregnant?
Insulin is injected into your fatty tissue. The picture below shows the places on your body that can be used. The best place to use during pregnancy is your abdomen (stomach, belly). You can use your arms or legs if you cannot use your abdomen.
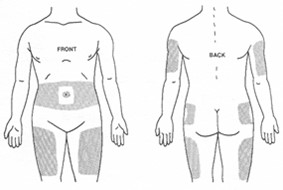 Abdomen (stomach)
Abdomen (stomach)- The insulin gets into the blood stream faster than other places.
- Stay 2 inches away from the belly button.
- You can inject above or below the waist.
- Arms
- Measure 1 hand width down from the shoulder and 1 hand width up from the elbow.
- Inject into the fleshy, outer surface.
- Legs
- Measure 1 hand width down from the groin and 1 hand width up from the knee.
- Inject into top and outer part of the leg.
- Do not inject into inner thigh.
- Buttocks
- Inject into upper, outer area of the buttocks.
Tips
- Do not inject into scars, bruises, or sores.
- Rotate injection sites within 1 chosen area of your body.
What is hypoglycemia (low blood sugar)?
It is when the sugar level in your blood is too low. In pregnancy, a blood sugar below 60mg/dl is too low.
Causes of a low blood sugar are:
- Taking too much diabetes medicine.
- Not eating enough food or delaying meals or snacks.
- Waiting too long to eat after you take your medicine.
- Exercising more often or for longer than normal.
Signs of a low blood sugar are:
- Shakiness
- Sweating
- Feeling nervous
- Feeling hungry
- Feeling dizzy or faint
- A racing (fast) heart
- A headache
- Feeling impatient
- Being confused
- Feeling cranky
- Blurred vision
- Slurred speech
- Numb lips or tongue
Treat a low blood sugar by:
- Testing your blood sugar.
- If your sugar is less than 60 mg/dl it is too low.
- Eating or drinking 15 grams of carbohydrate. Some choices are:
- Fruit juice (1/2 to 3/4 cup, 4 to 6 ounces
- Non-diet soft drink/soda/pop (1/2 to 3/4 cup, 4 to 6 ounces)
- Skim milk (1 cup or 8 ounces)
- Honey/jelly/sugar (1 Tablespoon)
- 5 Lifesavers or 6 jellybeans
- 4 glucose tablets
- Retesting your blood sugar in 15 minutes.
- Repeat step 1 if your sugar is still less than 60 mg/dl.
- Eating a snack or meal within 30 to 60 minutes after a low blood sugar.
- If it is going to be longer than 30 to 60 minutes until your next meal or snack, you need to eat or drink an extra 15 grams of carbohydrate and a protein.
How do I get rid of my syringes and needles?
It is best to put your syringes and needles in a container that is used only for this purpose to prevent injury, illness, and pollution. Use a coffee can or hard plastic bottle, such as an empty bleach or liquid detergent bottle.
Do not use a container:
- That will be returned to a store or recycled
- Is glass
- Is clear plastic
Seal the lid with heavy-duty tape when the container is full.
Call your local waste department to learn how to get rid of your used syringes safely.
Do not take used lancets, insulin syringes, or needles to the hospital.
Keep all sharp objects out of the reach of children.
Call your care team if you have questions or concerns:
- Monday through Friday from 8:00 a.m. to 4:30 p.m.
- The Obstetrics and Gynecology Clinic at 319-356-2294. Ask for a Diabetes Nurse Clinician.
- For urgent questions or concerns on nights, weekends, and holidays call the hospital operation at 319-356-1616.
- Ask to speak with the gynecology resident on call.
- Send a MyChart message to the OB diabetes provider if your question is not urgent and is related to your diabetes.
- Please call if you have an urgent concern. Do not send a MyChart message. You will not get a response to MyChart messages on nights, weekends, or holidays.