UI Health Care offers these transfeminine gender-affirming genital surgeries:
- Bilateral orchiectomy
- Zero-depth vaginoplasty
- Full-depth vaginoplasty
This guide explains each of these procedures and includes:
- Descriptions of each procedure
- Instructions for how to prepare for each procedure, including information about letters of consent and hair removal
- Information what to expect in the days and months after your procedure, including medications, cleansing instructions, and guidelines for dilation of the vaginal canal (for full-depth vaginoplasty)
This removes both testicles. It happens through 1 incision in the middle of the scrotum.
This may be done in the office while you are awake. Local genital anesthesia is given. It may also be done in the operating room. In this case, you are monitored or given general anesthesia.
- It takes about 45 minutes.
- You will go home the same day.
- Your sutures will dissolve on their own.
- You will need a driver.
Medicines
- Pain relief such as:
- Tylenol
- Non-steroidal anti-inflammatory (NSAIDs)
- No antibiotic is needed.
- You may stop spironolactone right away.
Follow-up
- You will be seen in the urology clinic as needed.
- Follow-up with your hormone specialist. Some of your medicines may need to be changed.
This is the creation of external female genitalia without the vaginal canal. Orchiectomy can be done before or at same time of zero-depth vaginoplasty.
- It takes about 6 hours.
- People often go home 3 days after surgery.
- Your sutures will dissolve on their own.
Medicines
- Pain relief, such as:
- Tylenol
- Non-steroidal anti-inflammatory (NSAIDs)
- Opioid pain medicine can be taken as needed.
- You will take an antibiotic while you have a urinary catheter in place.
Wound care
- Put triple antibiotic ointment on the clitoris and urethra. Do this 3 times each day for at least 2 weeks after surgery.
- Put petroleum gauze or gauze with triple antibiotic ointment between the urinary catheter and clitoris. This stops the catheter from rubbing.
- After the catheter is taken out, you do not need to use gauze.
Follow-up
- Your care team will take the urinary catheter out about 2 weeks after surgery.
- After the catheter is out, you will follow-up at: 1 month, 3 months, 1 year.
Urination
Expect spraying of urinary stream when the catheter is taken out. This happens as the tissue heals and sutures dissolve. Spraying often gets better over time.
Sexual health
You may have more or less sensation to the clitoris after surgery as the nerves heal. Changes in sensation can take months to improve. You may start stimulating the clitoris 1 month after surgery.
This is the same as the zero-depth vaginoplasty except with the creation of the vaginal canal. Full-depth vaginoplasty (unlike zero-depth) requires genital hair removal before surgery and vaginal dilation after surgery.
UI Health Care offers penile inversion vaginoplasty using scrotal and penile shaft skin. Peritoneal pull-through and sigmoid vaginoplasty are not offered.
Orchiectomy can be done before or at same time of full-depth vaginoplasty.
- It takes about 6 hours.
- You will be on bedrest for 5 days.
- You will go home 5 days after surgery.
- Your sutures will dissolve on their own.
Medicine
- Pain relief, such as:
- Tylenol
- Non-steroidal anti-inflammatory (NSAIDs)
- Opioid pain medicine can be taken as needed.
- You will take an antibiotic while you have a urinary catheter in place.
Wound care
- Put triple antibiotic ointment on the clitoris and urethra. Do this 3 times each day for at least 2 weeks after surgery.
- Put petroleum gauze or gauze with triple antibiotic ointment between urinary catheter and clitoris. This stops the catheter from rubbing.
- After the catheter is taken out, you do not need to use gauze.
Follow-up
- Your care team will take the urinary catheter out about 2 weeks after surgery.
- After catheter is taken out, you will follow-up at: 1 month, 3 months, 1 year.
Urination
Expect spraying of urinary stream when the catheter is taken out. This happens as the tissue heals and sutures dissolve. Spraying often gets better over time.
Sexual health
You may start stimulating the clitoris 1 month after surgery. Do not have penetrative intercourse for at least 3 months.





Letters of support
You will need to get 2 letters of support from mental health providers. We cannot use recommendations from primary care providers. You must have these letters within 12 months of planned gender-affirming genital surgery. You may need to get new letters after a surgery date is planned.
New Leaf Counseling
910 23rd Ave., Suite 100
Coralville, IA 52241
319-351-9731
Clock, Inc
4102 46th Ave.
Rock Island, IL 61201
309-558-0956
Ellen Hallin Life Strategies
640 and 720 Walker Circle
Iowa City, IA 52245
319-601-0313
Seashore Psychology Clinic
335 E. Jefferson St.
Iowa City, IA 52242
319-335-2467
psychology.uiowa.edu/seashore-clinic
The Lindquist Center
240 South Madison St.
Iowa City, IA 52240
319-335-5500
When your paperwork is done, send an email asking for the appointment you need — for example, an ongoing psychotherapy assessment for a letter of support. Also give them your weekday availability.
Referrals will be made by the UI Health Care LGBTQ Clinic ([email protected]), if needed.
Resolute Therapy, LLC
1661 Boyson Square Dr., Suite 200 D
Hiawatha, IA 52233
319-210-8093
Other sources
Find a mental health facility close to where you live.
Letters of support need to include:
- Gender identity and history of gender dysphoria
- Meaningful close relationships and support of gender identity/transition
- Mental health history
- Substance use history
- Support in work environment
- Coping strategies
- Understanding of risks and benefits of surgery
Genital hair removal
People who want full-depth vaginoplasty need permanent genital hair reduction from the scrotum and penile shaft before surgery. Providers at the University of Iowa Health Care Dermatology Clinic offer laser hair removal. They do not offer electrolysis. Hair laser or electrolysis can be done wherever you prefer.
Genital hair removal is not needed before orchiectomy or zero-depth vaginoplasty.
Hair laser can be done safely on all skin types.
The hair laser targets pigment in the hair follicle. This means it only works for pigmented hairs. It does not work for light blonde, white, or fine hairs. People with a lot of blonde or white hairs may need electrolysis.
Hair laser only targets hairs in certain growth cycles. For best results, you may need hair laser every 4 to 8 weeks over 6 to 12 months.
People’s timelines can differ based on their response to the laser and settings used. These vary based on a person’s skin and hair type.
As you reach the end of hair laser treatment, you should not have regrowth of dark pigmented hair between sessions. If you have blonde or white hairs, you may need electrolysis. Your provider will talk with you and your surgeon.
Reach out to your surgeon near the end of hair removal. An office visit will be scheduled. Then a surgery date can be planned.
It is best to wait 1 full hair cycle (6+ weeks) before having a full depth vaginoplasty. This is to be sure there is no hair regrowth.
There can be mild to moderate discomfort. This is often better by the end of the day. You can use ice packs, acetaminophen, and topical anesthetics. The provider will talk with you about this if needed.
There will be redness. This is often better in 24 hours. Bruising and mild swelling can also occur. These are less likely.
Burns and blistering are rare. Call your provider right away if you notice this. Hyperpigmentation (darkening of the skin) and hypopigmentation (lightening of the skin) are also rare. If you notice this, it is often temporary. It can be permanent for some people.
Before your start, do not:
- Wax
- Pluck
- Use body sugar
- Use any chemical hair removers
Shave or trim the hair on the day of, or one day before, each treatment. Then only a small part of the hair shaft is above the skin.
Sites that need to be treated are the scrotum, penile shaft, and about 2.5 cm below the scrotum (perineum).
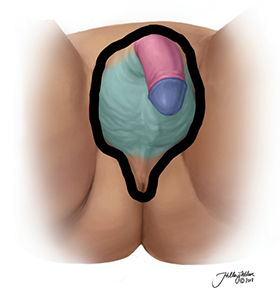
Hair laser treatment should remove hair from the sites surrounded by a thick black line — the scrotum, penile shaft, and about 2.5 cm below the scrotum.
Hormone therapy
Before zero- or full-depth vaginoplasty, stop estrogen for 2 weeks if you have:
- Diabetes
- Heart disease, including high blood pressure and high cholesterol
- Are older than 50
Otherwise, take estrogen until you have surgery, unless your doctor tells you something different.
If on progesterone, keep taking it. No need to stop before or after surgery.
After surgery, you will not take estrogen while in the hospital until catheter is taken out. This is often about 2 weeks after surgery. You can stop spironolactone as soon as the testicles are removed.
Pelvic floor physical therapy
(For full-depth vaginoplasty only)
At least 1 pelvic floor physical therapy (PT) visit will be scheduled before surgery. This helps comfort with dilation of vagina after surgery.
Goals before surgery:
- Screen for and treat pelvic floor muscle dysfunction
- Learn pelvic floor muscle contraction and relaxation
- Learn and do stretches to help pelvic floor muscle relaxation
- Teach healthy pelvic floor muscle habits
- Gain relationship with pelvic floor physical therapist
- Get these supplies:
- Handheld mirror
- Vaginal dilators
- Lubrication
- Washing supplies
Goals after surgery (optional):
- Screen for changes in pelvic floor muscle dysfunction
- Re-learn pelvic floor muscle contraction and relaxation
- Ensure successful dilation
- Review:
- Dilation
- Lubrication
- Washing
- Address other concerns, such as:
- Constipation
- Sitting posture
Vaginal care after surgery
(For full-depth vaginoplasty only)
Buy and bring dilators, lubrication, and handheld mirror with you to the hospital. Bring these to all follow-up urology and pelvic floor physical therapy visits if you have concerns.
Dilators are very important after surgery. You must buy them before surgery.
Your care team suggests Soul Source GRS vaginal trainers. Get sizes P2, #1, #2, and #3. They are easily found online. Many people choose blue or green dilators as their goal size. Goal size can change as goals change.
Dilation should start as soon as vaginal packing is taken out. This is 5 days after surgery. Start in the hospital before going home. There may be some discomfort, stretch, or tenderness. Do not push past resistance or into pain.
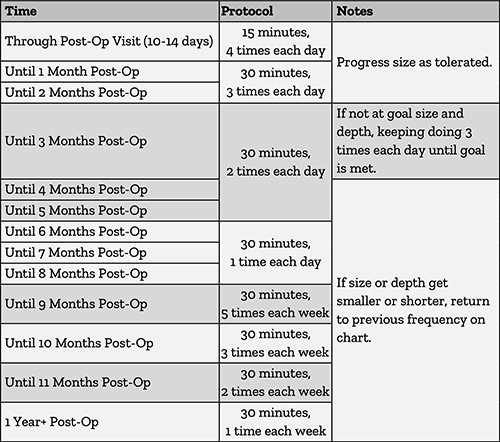
Dilation schedule
Easy: Insert to target depth. Takes less than 1 minute. There is little resistance or discomfort.
Medium: Insert to target depth. Takes less than 5 minutes. There is some resistance.
Difficult: Inserting takes more than 5 minutes. There is pain during or after insertion.
Try the next size after 3 easy sessions in a row. Split the session into 2 sizes for a total of 30 minutes. This can ease the change between sizes. Keep the same number of dots (depth) with all sizes.
Do not push past moderate resistance or into pain. Mild discomfort or stretching is normal.
Position and set-up
- Lie on your back with knees slightly open and supported.
- Use large amounts of medical-grade water-based lubrication, such as:
- Surgilube
- McKesson
- Medline E-Z
- After 3 months, switch to thinner, water-based lubricants, such as:
- Sliquid
- Slippery Stuff
- Astroglide
- A hand mirror can help lead you.
- Put the dilator in at a 45-degree angle with the dots facing you. This lets the dilator move under the pubic bone. When it is under, straighten the dilator to a flat angle.
During dilation
- Expect a small amount of resistance and tenderness with insertion. Stop when you feel moderate resistance and pressure.
- See how many dots are on the outside. Keep the same depth for the session.
- If you have trouble moving up sizes or feel tightness, slightly and gently tilt the dilator for pelvic muscle release.
After dilation
- Wash with gentle soap and water.
- Wipe from front to back to avoid infection.
- You may have some bleeding. It should slow and stop on its own. Call your care team if you bleed a lot.
- Call your care team if you think you have an issue or infection. Keep dilating unless told otherwise.
Lubrication
- Put a large amount on the dilator.
- Use water-based lubrication.
- Do not use silicone-based lubrication, oils, or thin water-based lubrication for at least 3 months after surgery.
- Lubrication will drain out from vagina after insertion. This is normal.
For zero- and full-depth vaginoplasty:
- Bilateral orchiectomy (if not done before)
- Partial penectomy
- Clitoroplasty
- Vulvoplasty: Creation of labia for zero and full depth vaginoplasty
- Urethroplasty
- Vaginoplasty: If undergoing full depth vaginoplasty
Risks:
- Bleeding
- Infection
- Deep venous thrombosis (blood clot in a deep vein)
- Abnormal urinary stream
- Abnormal sensation of clitoris
- Persistent gender dysphoria
- Desire for future labial revision
For full-depth vaginoplasty, other risks are:
- Loss of vaginal depth
- Vaginal stenosis (narrowing of vagina)
- Pain with penetrative intercourse
- Loss of vaginal graft
- Rectal injury