New eCPR program helps save Iowa man’s life
When traditional CPR wasn’t enough to restart Ken Platt’s heart after cardiac arrest, UI Health Care teams leaped into action to initiate extracorporeal cardiopulmonary resuscitation.

After waking up in the middle of the night with chest pain on March 9, 2024, Ken Platt was taken by ambulance from his Muscatine home to University of Iowa Health Care in Iowa City.
When his wife, Kaitlynn Platt, arrived at the hospital, she was told that Ken’s heart had stopped twice despite health care professionals performing CPR and using a defibrillator to deliver an electric charge to try to restore a normal heartbeat.
“The doctor told me there was one more thing they could try,” Kaitlynn Platt says. “I just remember saying, ‘Try whatever you can.’”
That “one more thing” was extracorporeal cardiopulmonary resuscitation (eCPR). UI Health Care launched its eCPR program in November 2023. It is the only eCPR program in Iowa and one of only a small number in the country — and Ken Platt was one of the first patients at UI Health Care to get it.
ECPR is a technique that uses extracorporeal membrane oxygenation (ECMO) on patients who have had cardiac arrest and for whom conventional CPR or a defibrillator has failed. During eCPR, a patient’s deoxygenated blood is removed from a central vein and passed through a membrane oxygenator, which removes carbon dioxide and adds oxygen to the blood. The blood is then returned to the body through the femoral artery.
“CPR wasn’t enough for me that night, so thank goodness they had that one more option,” Ken says. “I don’t think I would be here without that. The UI Health Care team was nothing short of amazing. They saved my life.”
A new approach to saving lives after cardiac arrest
More than 350,000 Americans experience cardiac arrest — when the heart suddenly stops beating — every year outside of a hospital setting. Even if a person is fortunate enough to have a bystander or emergency medical services immediately begin performing CPR, the rate of survival is only about 10% — a number that has not changed in decades. And if a patient has not been successfully resuscitated within 40 minutes from the moment they first collapsed, their chances of survival after that are almost zero.
A National Heart, Lung, and Blood Institute–funded study known as the ARREST trial, published in November 2020, showed how effective eCPR could be. In fact, the early results were so successful that the institute halted the study because outcomes for cardiac arrest patients who got eCPR were far superior to those receiving standard care. After six months, 43% of the patients who got eCPR were alive with good brain function, compared with zero in the control group who got standard advanced cardiac life support (ACLS) treatment.
“The whole world woke up to the success of ARREST trial,” says Lovkesh Arora, MBBS, MD, anesthesiologist and ECMO medical director at UI Health Care. “The ECMO leadership team at UI also started looking at how we can best deliver a successful outcome in these patients.”
There are almost 800 ECMO centers in the world, and the Extracorporeal Life Support Organization classifies UI Health Care’s program as one of only 43 platinum-level centers of excellence.
But not every health care facility that provides ECMO can immediately start an eCPR program. It took UI Health Care nearly two years of planning to start its program.
“It’s not one of these things where you can just snap your fingers and say, ‘Hey, we’re going to have this,’” says Phillip Horwitz, MD, a cardiologist and executive director of UI Health Care’s Heart and Vascular Center. “It requires an institution that has a uniquely high level of expertise, which is few and far between. It requires a collaborative effort between a lot of different services: ambulance services, emergency room staff, cath lab teams, interventional cardiologists, cardiac surgeons, cardiac ICU, ECMO management physicians, and ECMO specialists. All these specialists are required to manage one of these patients, so it really can only be done at a large tertiary care center that has the resources and is willing to dedicate those resources to something like eCPR.”
ECPR will not cure a patient. But by providing good blood flow to the brain and other organs, eCPR allows the body to rest and provides doctors time to treat the underlying problem.
For eCPR to have a chance at saving a person’s life, evidence suggests that it must be started within an hour after the event begins.
“Every second is like gold,” Arora says. “There is no room to waste time, as we need to do everything from patient transport to ECMO initiation within those 60 minutes from the time of witnessed arrest, so we have developed a workflow where once a designated physician activates eCPR, things move fast and efficiently to achieve that goal.”
Horwitz says the eCPR program allows them to help save more lives.
“There are people like Mr. Platt who come here critically ill. And if he went to any other institution in the state, he wouldn’t have survived,” Horwitz says. “For him to be able to walk out and have a fruitful and productive life, that’s what this program is for.”
Overcoming complications to return home
Ken Platt remained on ECMO for a week, during which time stents were inserted to open his blood vessels and a temporary artificial heart pump was placed to help support his weakened heart.
“I think he had seven procedures — minor and not — within seven days,” Kaitlynn Platt says. “It was boom, boom, boom, one thing after another.”
Ernesto Ruiz Duque, MD, a cardiologist at UI Health Care, says ECMO allowed him and his colleagues time to come up with a treatment plan.
“They saved his life, and they saved his brain when they put him on ECMO,” Ruiz says. “Then we worked to help him recover and become strong enough to go home and live his life.”

Ken doesn’t remember anything from the first month and a half of his 75 days at UI Health Care. But Kaitlynn remembers all of it.
“Dr. Arora encouraged us to take it one day at a time, which was hard,” Kaitlynn says. “One of the most stressful moments was when they lowered the power of the ECMO before taking him off it. There was complete silence as everyone watched the machine and his vitals and made sure that his body was going to be able to do what it needed. I remember Dr. Arora telling us that once it comes out, it will not go back in. So, they had to be sure that things were going the way they needed to.”
Ken was weaned off ECMO seven days after going on it.
“As with the importance of timely escalation of support with ECMO therapy, timely de-escalation from these mechanical circulatory support devices is also crucial, as every day on these devices adds to more complications,” Arora says.
Ken faced multiple setbacks during his time in the hospital. His care team included specialists from cardiology, the transplant center, gastroenterology, and infectious diseases, among others.
“It seemed like whatever could go wrong with him medically did,” Kaitlynn says. “But Ken never worries about himself; he always worries about everyone else but himself. At one point, they were getting ready to tube him and he kept asking where my son was. He could hardly breathe and that’s what he was worried about.”
Ruiz says Ken’s heart was so weak that the original artificial heart pump they placed was too small, so they had to replace it with a bigger one.
“It was used as a bridge until we knew if his heart would heal fully or if he would need a transplant or something else,” Ruiz says.
The left ventricle of Ken’s heart did not recover. Because he was not a candidate for a heart transplant, it was decided that he would get a permanent, surgically implanted mechanical heart pump known as a left ventricle assist device (LVAD).
Before he could get approved for an LVAD, however, Ken had to work with a physical therapist to gain back some strength and mobility.
“He was still in a lot of pain and didn’t really want to walk,” Kaitlynn says. “But Dr. Arora visited and basically told Ken to suck it up. The next day Ken did a lap around the unit.”
Ruiz says patients sometimes need a little tough love, and he joined his colleague in encouraging Ken to get up and move.
“Treatment requires more than pills,” Ruiz says. “I am there to tell the truth. I encouraged him to think about his family and the things he was missing. I told him he had a chance to recover from this if he worked harder. And he did, and that’s why he’s doing so well right now.”
Extracorporeal membrane oxygenation (ECMO) is a life support therapy. It’s used if you’re critically ill with heart failure or lung failure and other treatments aren’t working.
The UI Health Care Heart and Vascular Center is internationally known for ECMO expertise and has been named a Platinum Level Center of Excellence. Our experts train medical professionals from all over the world in how to use ECMO.
Arora says it’s not easy being in the ICU for so long, and it’s not unusual for patients to feel down.
“The Platts are such lovely people, and they went through a lot,” Arora says. “It’s very rare to see a patient like Ken who stayed so positive throughout. It not only helps the patient, but it also helps the care team to see someone in such full spirits.”
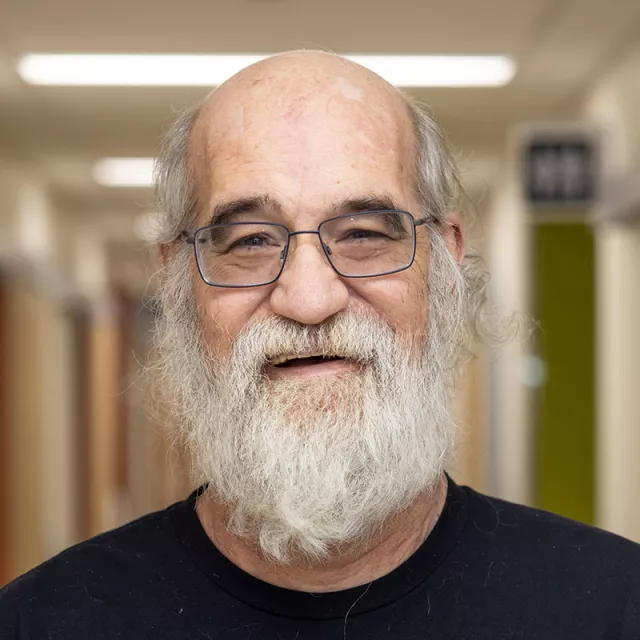
Ken credits one especially important aspect to his recovery: “I don’t know if I would have pulled through this if it wasn’t for my family.”
Along with Kaitlynn, Ken’s children, Amber and Austin, spent countless hours at the hospital with Ken. And on the days when one of them wasn’t there, they were getting frequent updates from the family members who were.
“I may be next of kin, but I didn’t make any decisions unless we all spoke,” Kaitlynn says. “We all leaned on each other.”
Ruiz agrees that having a strong support system is important.
“I have seen that when family is there providing support, the outcomes are better,” Ruiz says. “His family was with him all the time, and I think that was a key part of his recovery.”
One of the first few days in the hospital, Kaitlynn had to do something she told Ken she’d never do.
“He had an amazing beard that was never, ever to be cut,” Kaitlynn says. “But they had to shave him in case they needed to put a catheter in his neck.”
“For the first split second I was upset,” Ken says about first seeing his clean-shaven face. “But the doctor said we had to do it, and I trusted them. And it’s growing back now.”
Ken and Kaitlynn had been married less than a year when Ken was hospitalized.
“She told me, ‘Well, you took “in sickness and in health” literally,’” Ken says, laughing.
As Ken prepares to begin outpatient cardiac rehabilitation, Kaitlynn says it’s amazing to see how far he’s come.
“So many nurses and even doctors have told us that they didn’t know if he was going to pull through; that he is a miracle,” Kaitlynn says. “Looking back, I can see that!”
Ken says he’s thankful for the many care providers who made it possible for him to return home to his family.
“I’m just glad I was brought to Iowa City,” Ken says. “I wouldn’t have made it if I was taken somewhere else.”
Patient Stories

