Under the leadership of Dr. Mohammad Amarneh, an experienced team of physicians and nurses at University of Iowa Hospital & Clinics has been offering Selective Internal Radiation Therapy (SIRT) for inoperable liver cancer since 2004.
What is Y90 Radioembolization (SIRT)?
Radioembolization, also known as Selective Internal Radiation Therapy (SIRT), is a form of internal radiation therapy used in certain patients who are not candidates for surgery or percutaneous ablation of their liver tumors.
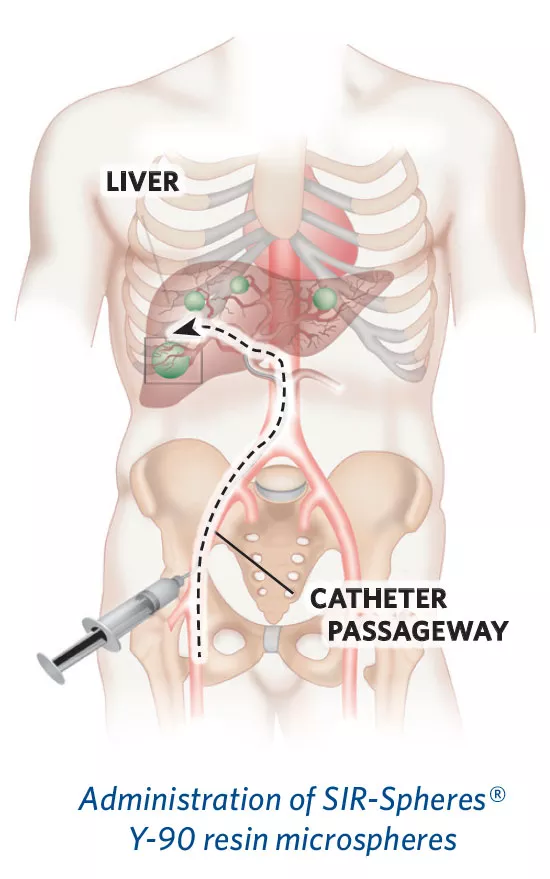
Beads coated with yttrium-90 (Y90) are delivered to the tumors in the liver through the arteries supplying the liver. Y90 is a beta-emitting radionuclide that acts locally at the tumor site. The beta particles emitted travel up to 11 mm in the liver. This allows the beads to irradiate the tumor while sparing healthy liver tissue. Additionally, given the short distance it travels, there are minimal, if any, necessary radiation safety precautions following treatment.
These radioactive beads, also called microspheres, target liver tumors by taking advantage of the increased arterial blood flow to the tumors. Normal liver tissue, on the other hand, is predominantly fed by the portal vein.
We offer both SIR-Spheres and Therasphere, the only two types of microspheres currently available for treatment.
Who is involved in recommending and performing the treatment?
Usually the patient’s oncologist will recommend that the patient consult with an interventional radiologist for radioembolization. Our Interventional Radiology team collaborates treatment with referring physicians and other medical specialties at University of Iowa Hospital and clinics, which include Medical Oncology, Liver Transplant, Surgical Oncology, Radiation Oncology, as well as oncologists in the community.
of Sirtex SIR-Spheres Pty Ltd.
How is SIRT performed?
The radioembolization treatment is performed as an outpatient procedure by interventional radiologists. During the procedure, the radiologist inserts a catheter into the artery in the groin and guides it to the arteries supplying the liver using live X-ray. The radioactive particles are then administered to the area of the tumor.
Once the beads are administered, the therapeutic dose of radiation is delivered over a period of two weeks.
The treatment normally takes about 60 to 90 minutes, with most patients returning home four to six hours later. Patients are carefully monitored throughout and after the procedure. The most commonly reported side effects are flu-like symptoms over one to three weeks. The procedure can be performed in combination with chemotherapy or by itself.
After the procedure, patients are placed on bed-rest for two to six hours. Most patients are able to go home the same day.
How effective is SIRT treatment and are there any side effects?
Clinical studies have shown that SIRT increases the length of time that the cancer is stable and not growing without adversely affecting the patient's quality of life. In several clinical studies, the SIRT procedure has been combined with chemotherapy, given as a single procedure during a chemotherapy holiday or after chemotherapy options have failed. These patients have demonstrated increased survival and longer time to disease progression.
Overall the treatment is very well tolerated with minimal side effects. The most common side effect is fatigue, which can last two to four weeks.
In rare instances, a small number of microspheres may inadvertently reach other organs in the body, such as the gallbladder, stomach, intestine, or pancreas. If microspheres reach these organs, they can cause inflammation or ulceration. These complications are rare, but if they do occur they will require additional medical treatment. These complications are often avoided by performing a procedure prior to radioembolization that identifies and blocks arteries to these other organs, preventing the microspheres from reaching them.
Do patients have to take special precautions and when will I receive the results?
There are some simple precautions that patients need to take during the first 24 hours following the SIRT procedure. These precautions include: thorough hand washing after using the toilet; and cleaning up any spills of body fluids such as blood, urine or stools and disposing of them in the toilet. Otherwise, patients can resume normal contact with family members.
The interventional radiologist will be able to inform you whether the procedure was technically successful. Your oncologist will order follow-up imaging to determine the clinical success of the procedure and whether additional procedures or treatments may be necessary.
Locations and Offices
